Medical Billing / Revenue cycle management require a vast knowledge of coding, billing, and payer rules.
Managing revenues in-house leads to high-costs & giving less time for patient care, particularly for smaller practices.
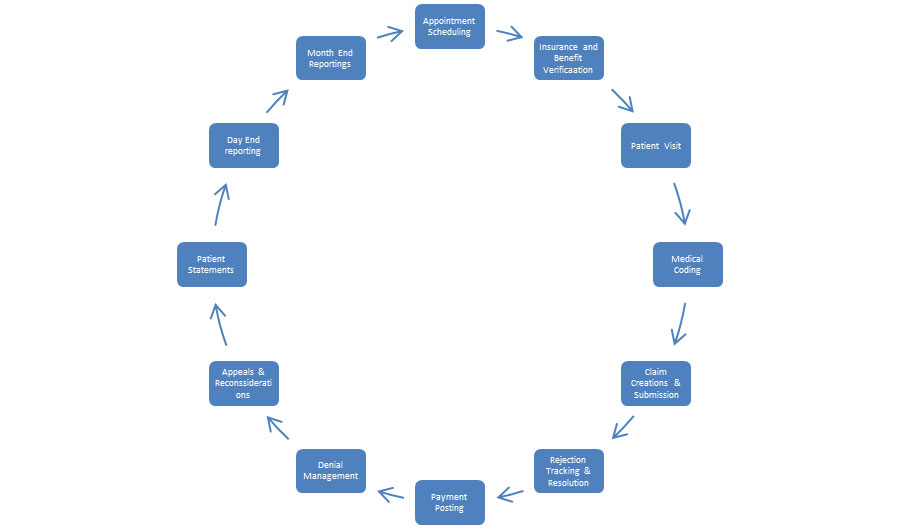
Services Provided at PAMM Infotech
Provider and Outsourcing unit share a very close bond. Provider only has to focus on providing quality services to patient whereas all the back end operations are taken care by PAMM Infotech
Charge Entry and Payment posting
Provider Credentialing & EDI Set up
Electronic and paper claims submission
Denial and A/R management
Preparing Appeals / Reconsideration & Follow Up
Insurance & Collection Agency follow ups & Collections
Patient Statements & Collections
Month End Reporting
PHI ( Protected Health Information):-
This includes identifiable demographic and other information relating to the Patient physical or mental health to be kept fully confidential. For purposes of the Privacy Rule, genetic information is considered to be health information. Proper security will be in place so that patient information is not shared out.
EDI Setup:-
We have an experienced staff who specializes in EDI Contracts with the Insurance companies and the clearing house. This will eliminate all the Paper claims submissions & check that comes to Provider and the Payments are directly deposited in Provider bank accounts. This also helps lower the Manpower as Posting Insurance money along with the reconciliation is just few click away.
REDUCED PAPER WORKFLOW:-
This was observed that provider who doesn’t have experienced staff that can work on Electronic Data Setup has a delay in submitting claims to Insurance company which leads to delay in receiving Payment. In past when claims were mailed to insurance companies, Provider’s kept on waiting for payment to come in thru Insurance Via Paper check for approximate 35-40 days but we have an experienced staff who guarantee 90% of claims to be submitted electronically which makes claims to land at insurance door steps within 48 Hours and with setting up ERA/EFT contracts with insurance companies, the payment comes directly into provider bank account within 15-18 days.
Denial Management:-
CMS publishes guidelines for provider telling them which services according to their specialties will be reimbursed or not, so on an average Provider 30-40 % of revenue is denied upfront by Insurance companies for ABC reason. Compiling 30-40 % of denial volume for current months & LAST month added land Provider in Very BAD situation, so experienced staff with TOP Most analytical skill set can work on denial trending, find out the resolutions and can even present the Excel tracking to Provider anytime. This means outsourcing unit is always ready with financial analysis for Provider & in same way they work out with insurance company to collect the revenue.
Aging Capture:-
By word Aging we Means the average age of claim. In today’s RCM world we have 5 major type of insurance type classified as FINANCIAL CLASSES as listed below. Each Financial class has their timelines & guidelines to pay. The rules /TAT of Claims processing are DIFFERENT for almost EACH class.
| Financial Classes |
|---|
| Medicare |
| Medicaid / Medicaid |
| Managed Care plan (PPO /HMO/Commercial insurances) |
| Worker’s Compensation |
| PrivatePay / Self pay |